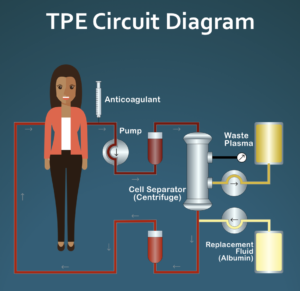
 Recently, we have been getting an increasing number of inquiries about the use of Therapeutic Plasma Exchange (TPE) as a potential treatment for systemic sclerosis (SSc). If any of you are unsure what we are talking about, start by watching this video: https://youtu.be/iWT0oW8FRdE. It is targeted at clinicians but is pretty easy to understand.
Recently, we have been getting an increasing number of inquiries about the use of Therapeutic Plasma Exchange (TPE) as a potential treatment for systemic sclerosis (SSc). If any of you are unsure what we are talking about, start by watching this video: https://youtu.be/iWT0oW8FRdE. It is targeted at clinicians but is pretty easy to understand.
A number of new questions have come up recently, so we thought this post might be useful in answering them.
- Who can order TPE? Does it have to be a rheumatologist? While the specifics will depend on the policies of the clinic/hospital, any MD or equivalent can order TPE. It does not have to be a rheumatologist. The first physician to try our recommended TPE protocol on an SSc patient (in Europe) is a hematologist. (Note: TPE is a commonly used treatment for some blood disorders typically treated by hematologists.) In the US, a Functional Medicine MD is planning on trying TPE with an SSc patient early next year.
It is important to understand that TPE is a routine medical treatment for a number of disorders, but is not currently a routine treatment for SSc. Using TPE to treat SSc is an “off label” use of TPE. (As a side note, all drugs commonly used as systemic treatments for SSc like methotrexate, Cellcept, and Rituxan are not approved by the FDA as treatments for SSc and are being used “off label” as well.) - What is the recommended protocol for a trial of TPE and why is this specific protocol recommended? The recommended protocol for a one-year trial of TPE is one treatment per week for four weeks followed by eight weeks of rest. This sequence is then repeated for a total of 16 treatments during the one-year trial period.
Here is background information on why this protocol is suggested. As early as 1979, SSc researchers noted that all of the symptoms seen in SSc, including fibrosis and systemic organ damage, appear to start with damage to the layer of cells that lines all blood vessels (endothelium). In the late 80s and early 90s, research was done (mostly in the Netherlands) that documented that blood rheology (physical characteristics of blood) is highly abnormal in patients with SSc. Overall blood viscosity (thickness) is elevated and red blood cells are clumped together abnormally. In 1993, after reading this little-known research, we hypothesized that if some of the red blood cell clumps are small but tightly bound, this could potentially cause trauma to the endothelium over time, since the smallest blood vessels normally allow only one red blood cell at a time to pass through. This damage to the endothelium could in turn lead to fibrosis and the entire downstream symptom cascade seen in SSc, as suggested by earlier researchers.
Other related research done at the same time documented that a series of weekly TPE treatments gradually improved blood rheology, and after four weeks, it was completely normal. Typically, symptoms such as Raynaud’s resolved and digital ulcers began to heal. Surprisingly (to the researchers), blood rheology returned to the abnormal, pre-TPE state very slowly. Even three months later, red blood cell clumping levels were only half of what they were before the series of four weekly TPE treatments. By nine months, blood rheology was back to pre-treatment levels, but, unfortunately, the researchers did not test between three and nine months so we have no data as to when blood rheology regressed to pre-treatment levels.
The treatment protocol we are suggesting, which we are calling “pulsed plasma exchange” is entirely based on this research. The treatment model is simple. Our current hypothesis is that by normalizing blood rheology, including eliminating potentially damaging red blood cell clumps with a series of four weekly TPE treatments, further damage to the endothelium is stopped or greatly slowed down. Then, since blood rheology remains normal or close to normal over the next eight weeks, additional damage is kept to a minimum, allowing the body to heal to the extent possible. The best way to think about this pulsed TPE protocol is that it is designed to always keep someone with SSc on the verge of further disease progression, without actually getting there. There is much more background information on abnormal blood rheology in SSc in the Research section of this website.It is important to understand this is a working hypothesis at this point. While there is extensive research suggesting that TPE is often beneficial to patients with SSc, there is currently only one published case report where this exact protocol has been used to treat a patient with SSc (for 22 years at the time of publication). We are planning on submitting a second case report for publication on a patient using this pulsed TPE protocol sometime early next year.
- How long do you need to continue TPE if it is “successful”? SSc is a chronic, life-long disease. With the possible exception of autologous stem cell transplants (HSCT), any treatment used for SSc, whether TPE or commonly used immunosuppressants like methotrexate or Cellcept, has to be continued indefinitely to remain effective. Our hope is that future research on TPE may lead to a full understanding of how and why it appears to works for as long as it does. With this knowledge, this in turn may lead to alternative treatment approaches to TPE that have the same or greater benefit.
- I live in a rural area that is not close to a major hospital –is TPE an option? We strongly recommend that anyone considering a trial of TPE should have this done at an infusion center at a major hospital where TPE is a routine outpatient procedure that is done several times a day. At a center like this, the infusion center nurses will have experience dealing with everything from venous access problems to potential problems that might come up during a treatment. A typical treatment takes about 2 1/2 hours from the time you arrive until you would be ready to go home. Since the protocol that we are suggesting requires 16 visits per year on an ongoing basis, you would need to consider travel time and other issues in making a decision to start a trial of TPE.
- I live outside the US. Here, most therapeutic apheresis is mostly done using a membrane filtration system rather than a centrifugal blood separation system as you recommend. Is this type of system likely to be effective? Unfortunately, there is very little research to answer this question. Two of the 46 studies that we reviewed used membrane apheresis systems and both showed benefit. There are many different ways to do filtration apheresis, which is an additional problem. Unlike centrifugal TPE, we have no data that suggests how effective these types of systems are at normalizing blood rheology, so we do not know if a completely different protocol would be required to achieve the same benefits. For this reason, we cannot recommend trying our protocol with filtration apheresis systems.
