 This morning, NPR did a report on dangers associated with long-term use of proton pump inhibitors such as Prilosec (omeprazole) and also the fact that it is nearly impossible to get off them. Here is a link to the article on their website: http://www.npr.org/sections/health-shots/2016/02/15/465279217/popular-heartburn-pills-can-be-hard-to-stop-and-may-be-risky. This is a very important story but people with systemic scleroderma need to realize that sometimes the rewards outweigh the risks and that you should not try stopping these meds on your own without talking with your doctor (you probably won’t be successful in any case for reasons mentioned in the article). The article does cover a number of important topics and mentions that PPIs can lead to things like magnesium deficiencies or deficiencies of other nutrients. These types of problems can easily be dealt with. Other long-term risks are mentioned as well.
This morning, NPR did a report on dangers associated with long-term use of proton pump inhibitors such as Prilosec (omeprazole) and also the fact that it is nearly impossible to get off them. Here is a link to the article on their website: http://www.npr.org/sections/health-shots/2016/02/15/465279217/popular-heartburn-pills-can-be-hard-to-stop-and-may-be-risky. This is a very important story but people with systemic scleroderma need to realize that sometimes the rewards outweigh the risks and that you should not try stopping these meds on your own without talking with your doctor (you probably won’t be successful in any case for reasons mentioned in the article). The article does cover a number of important topics and mentions that PPIs can lead to things like magnesium deficiencies or deficiencies of other nutrients. These types of problems can easily be dealt with. Other long-term risks are mentioned as well.
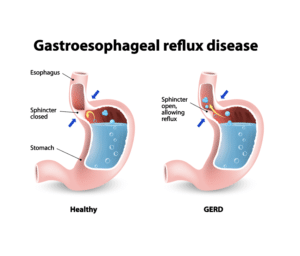
However, with systemic scleroderma, almost all patients will develop GERD because the lower esophageal sphincter becomes weakened through fibrotic processes inherent in scleroderma. Usually this leads to intense heartburn pain, but in some cases the reflux can be silent but still very damaging. For example, a particularly dangerous situation can occur where patients have so much damage to their esophagus that they may no longer feel pain because the nerves are damaged. If they stop taking PPIs, they may feel fine but still be suffering from reflux that might lead to serious complications such as Barrett’s Esophagus, a pre-cancerous condition. This is why it is critical that you consult with your doctor if you have concerns about long-term usage of PPIs.
There are, in fact, legitimate situations where people no longer need a PPI and need to know how to get off this type of medication without experiencing a major rebound effect. For example, my wife was on PPIs for a while because she developed an ulcer. After she was successfully treated for her H. Pylori infection that caused her ulcers, she could not get off them either. Every time she tried to stop taking Prilosec, she developed heartburn again immediately. Here is why: a study done in 2009* (see reference below) showed that if you put healthy volunteers with no heartburn problems on PPIs, they actually develop heartburn when you stop the PPIs! This is the ultimate medicine for a pharmaceutical company – it creates its own need!
In my wife’s case, we came up with a schedule to slowly taper her off the PPIs over 13 weeks and that worked perfectly. She had no rebound problem at all and has never needed PPIs again.
(As a side note, I had the same problem. When I went into remission from my limited scleroderma in 1996 following two years of plasmapheresis treatments, I tried to stop taking Prilosec but was unsuccessful for the reasons stated above. After my wife was able to successfully taper off her use of Prilosec over 13 weeks, I tried exactly the same thing and also was able to get off completely with no problems. It is actually very likely that I could have stopped taking Prilosec back in 1996 had we realized this!)
The bottom line is that for most people that have any variant of systemic scleroderma, untreated reflux can be a serious problem. If you have concerns about long-term use of PPIs, you should talk with your doctor about the risks and rewards from using them in your individual situation.
Reference
* Reimer C, Søndergaard B, Hilsted L, Bytzer P. Proton-pump inhibitor therapy induces acid-related symptoms in healthy volunteers after withdrawal of therapy. Gastroenterology. 2009;137(1):80-87.

Ruth, the fundamental concern about stopping PPIs as bad as they are is that there can be major problems from uncontrolled reflux, for example, Barrett’s, which can lead to esophageal cancer. The only reason that I was able to successfully taper off PPIs was that I had treated my underlying disease and my esophagus had completely healed so I haven’t had problems for many years. Without something that fundamentally alters the status of your underlying disease, e.g., TPE treatments or autologous stem cell transplants, which can (to a major extent) re-set the immune system, the judgement of the scleroderma experts that I talk to is that the tradeoffs suggest that being on PPIs is better than being off them, even with the significant potential risks of long-term use of PPIs.
I too have SSc Limited. I tried to stop the Prilosec as it can cause weakened bones even to the point of easy breaks. I thought I was having a heart attack from the heartburn but I stopped it cold turkey. I just don’t know if it was rebound reflux or what. How did you taper? I take 1 in am and 1 in pm before bed, 20 mgs. When it got bad for a while my GI Dr said to just double it. I did not. I started back up to the same dosage and I’m fine now. Please share your tapet schedule. The list of side affects is endless. Thank you so much! Ruth
Thank you for taking the time to post this thoughtful response to the article – and hopefully preventing knee-jerk reactions in some people who should not stop this medication without careful consideration and consultation with their physician. My mother had Systemic Scleroderma with chronic GERD which was very poorly managed. She had Barrett’s Esophagus and eventually underwent a complete esophagectomy for suspicion of cancer. The postoperative complications exacerbated by her Scleroderma led to her death at age 62. I have since been diagnosed with Scleroderma and have significant esophageal dysmotility and had constant heartburn prior to starting Proton Pump inhibitors twice daily . This NPR article could almost talk me into stopping them. Your post has helped put that into perspective.