 As more and more patients are now starting trials of pulsed therapeutic plasma exchange (PPE) as an experimental treatment for their diagnosed systemic scleroderma (SSc), I have noticed that in several recent cases, a hematologist has been added to the care team. The presence of a hematologist allows the rheumatologist who is typically heading the care team to feel more comfortable trying PPE. The reason is simple: therapeutic plasma exchange (TPE) is a routine treatment for a number of diseases, many of which are blood disorders. In contrast, rheumatologists rarely use TPE and frequently have an incorrect view that TPE is very risky and should be only used as a last resort if all other treatments fail. (In reality, TPE is very safe, MUCH safer than any immunosuppressant used to treat SSc.)
As more and more patients are now starting trials of pulsed therapeutic plasma exchange (PPE) as an experimental treatment for their diagnosed systemic scleroderma (SSc), I have noticed that in several recent cases, a hematologist has been added to the care team. The presence of a hematologist allows the rheumatologist who is typically heading the care team to feel more comfortable trying PPE. The reason is simple: therapeutic plasma exchange (TPE) is a routine treatment for a number of diseases, many of which are blood disorders. In contrast, rheumatologists rarely use TPE and frequently have an incorrect view that TPE is very risky and should be only used as a last resort if all other treatments fail. (In reality, TPE is very safe, MUCH safer than any immunosuppressant used to treat SSc.)
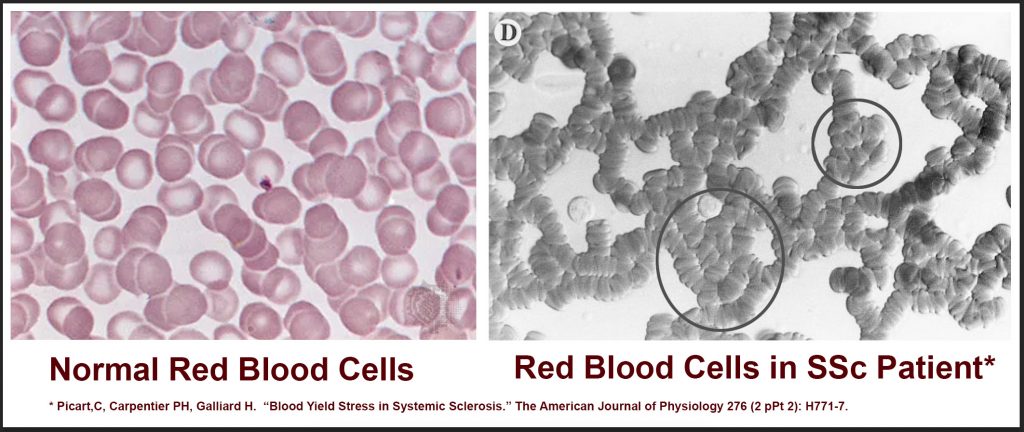
There is a significant body of research that documents that patients with SSc have very abnormal blood. The nature of this abnormal blood is that overall blood viscosity (blood thickness) is significantly elevated because red blood cells are abnormally clumped together. Some researchers believe that the abnormally clumped red blood cells in SSc patients contribute to damage to the inside of small blood vessels. Researchers now know that this early blood vessel damage is one of the earliest stages of the disease process in patients with SSc, later leading to fibrosis and systemic organ damage.
Hematologists are the primary specialists dealing with many blood-related diseases including a class of diseases call hyperviscosity syndromes. There are several different types of hyperviscosity syndromes, including variants where you have too many red blood cells, white blood cells, or blood proteins. There are also hyperviscosity syndromes where red blood cells are abnormally clumped together, although slightly differently than the red blood cell clumping seen in SSc. As it turns out, TPE is a treatment of choice for all hyperviscosity syndromes, so hematologists are very familiar with this treatment option.
TPE is correctly considered to be experimental when used as a treatment for SSc even though it is commonly used to treat other diseases. This means that when TPE is tried as a treatment for SSc, it is an “off label” use of a standard treatment. Note that all immunosuppressive drugs commonly used to treat SSc, including Cellcept (mycophenolate mofetil), methotrexate, and Rituxan (rituximab) are also “off label” uses of common drugs, as none of these are approved as a treatment for SSc either.
It should be noted that very few general rheumatologists are aware that blood in patients with SSc is abnormal. Some clinicians who commonly work with SSc patients are likely to be aware that SSc patients have abnormally thick blood, but in my experience, even many scleroderma researchers are completely unaware that the nature of the overall abnormal blood thickness is from clumped red blood cells.
This document (https://sclerodermainfo.org/pdf/PPE-Overview-US.pdf) was written for clinicians who are interested in a brief overview of pulsed plasma exchange. This article lays out a summary of the research and includes references for clinicians who want to learn more about this topic. It is not difficult to read, so I recommend reading it yourself if you have interest in this topic.
Bottom line: if you are interested in having an informed discussion with your rheumatologist about the possible risks and benefits of trying PPE to treat your diagnosed SSc, it will be helpful to also bring a hematologist into these discussions as they have a lot of expertise in TPE that your rheumatologist is unlikely to have.

No standard testing is available to measure red blood cell aggregation/clumping. Even whole blood viscosity is difficult to measure. You need to be near the lab that does whole blood viscosity measurement to do that test and many people will test in the normal range, according to the research on related measures such as sed rate (ESR). Whole blood viscosity is elevated in other diseases as well. Unfortunately, there is no trial going on currently for the PPE protocol. It is up to clinicians to try it on an individual basis.
Is there a test that recognizes the clumped red blood cells?
Is so, what is it called?
If not, how can it be proved that it exists?
I’ve been declining standard treatment so far so would like more information on TPE and how to take part in the trial.