 Recently, in a scleroderma focused Facebook patient support group, a newly diagnosed patient posted this comment after her initial doctor visit:
Recently, in a scleroderma focused Facebook patient support group, a newly diagnosed patient posted this comment after her initial doctor visit:
“…he told me that all they can do is chemotherapy when it starts taking over my body??? Really, is that it? Nothing they can do?”
Among many other supportive and helpful comments from other patients, one patient mentioned therapeutic plasma exchange (TPE) and described it as follows:
“They basically take out the plasma every few months or so and replace it. Like an oil change?”
While I had never thought of it that way (thanks Julie), it is actually an excellent analogy for what we think may be going on in systemic scleroderma and how TPE appears to lead to systemic improvements without suppressing the immune system.
Print Version – US: http://sclerodermainfo.org/pdf/TPE-Oil-Change-US.pdf
Print Version – A4: http://sclerodermainfo.org/pdf/TPE-Oil-Change-A4.pdf
Automobiles and Oil Changes
Cars use oil filters to keep the oil clean so that it stays at the best possible condition to keep your engine lubricated for maximum performance. If you don’t change your oil periodically, the oil gets “sludgy,” gradually leading to an overheated engine, poor performance, and in some cases, complete engine failure (sound familiar?).
Fortunately, most of us don’t need regular oil (blood) changes, since the body normally keeps our blood healthy so it can supply oxygen to cells and tissues, get rid of carbon dioxide, and fight infections. However, if you develop systemic scleroderma, everything changes.
Systemic Scleroderma and TPE: What We Know…
Here is some of what we know about scleroderma and therapeutic plasma exchange, based on published research:
- As far back as 1979, researchers realized that scleroderma is a disease that starts with damage to the inside of the smallest blood vessels from some type of repeated trauma. Once this damage occurs, it gradually leads to fibrosis and scarring, eventually causing organ damage throughout the body.
- Many research studies note that patients who are diagnosed with systemic scleroderma generally have abnormally “thick” blood compared to people who do not have an autoimmune disease. (Note: the medical term for blood “thickness” is “viscosity.”) One of the key components of this abnormally thick blood comes from red blood cells that are clumped together, which is not the norm. In healthy people, red blood cells are mostly separate from each other so they can flow easily throughout the body.
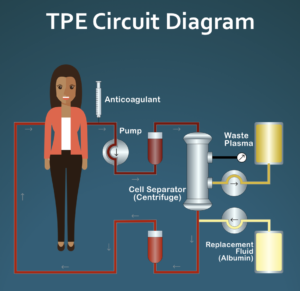
- Therapeutic plasma exchange (TPE/plasmapheresis) is a commonly used treatment for a number of different diseases, mostly autoimmune and metabolic disorders. Basically, TPE is a procedure where about two thirds of the liquid part of your blood (called your “plasma”) is replaced with a sterilized plasma substitute over about a 90 minute period. The idea behind this treatment approach is that it temporarily reduces the amount of any substances circulating in your blood that might be contributing to your disease, for example, destructive autoantibodies. TPE is a very safe procedure that is done in an outpatient setting over a 2- to 3-hour period in most cases.
Research has shown that a short series of TPE treatments has a significant effect on overall blood viscosity and red blood cell clumping. After four weekly TPE treatments, overall blood viscosity becomes normal and red blood cell clumping is gone. In addition, a number of research papers have noted that Raynaud’s symptoms are significantly improved or disappear completely and digital ulcers begin to heal as well.
Interestingly, if you do just one series of four weekly TPE treatments and then stop to see what happens next, these improvements in overall blood viscosity and red blood cell clumping last for a surprisingly long time. More on this in a bit…
Systemic Scleroderma and TPE: What We Think…
Note: While the rest of this article is consistent with published research, it should be considered to be speculative.
Here is what we think may be going on in systemic scleroderma and TPE.
Blood Vessels and Red Blood Cell Clumping
Normally, red blood cells flow through the smallest blood vessels one cell at a time. The average diameter of the smallest blood vessels is actually slightly smaller than the average diameter of a typical red blood cell. Because of this, red blood cells have to lengthen and fold to make it through the smallest blood vessels.
| Normal Blood Flow | 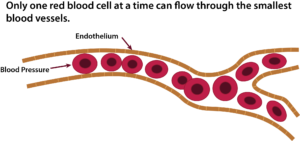 |
One of the early research studies that looked at the blood of scleroderma patients noted that the clumps of red blood cells did not break apart easily. Red blood cells do clump together in a number of different diseases, including rheumatoid arthritis and lupus. However, the type of red blood cell clumping in these diseases breaks apart very easily.
Consider what might happen if you have small clumps of red blood cells that are very resistant to breaking apart. Blood pressure may be able to force the red blood cell clumps through the smallest blood vessels up to a point; however, this could cause damage to the inside of the blood vessels over time. This could potentially be the cause of the “repeated trauma” to the blood vessels that leads to fibrosis and all of the organ damage seen in scleroderma that was discussed in the 1979 paper.
| Blood Vessel Damage | 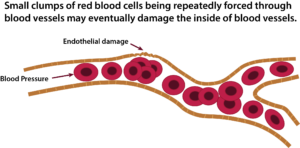 |
If these red blood cell clumps are larger than a few cells, then they could completely block blood flow in some of these tiny blood vessels.
| Blood Vessel Blockage | 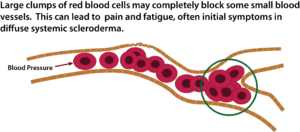 |
How TPE May Work
How does TPE affect red blood cell clumping? In 1991, a carefully done study (Jacobs 91) looked at how a series of four weekly TPE treatments modified overall blood viscosity and also red blood cell clumping.
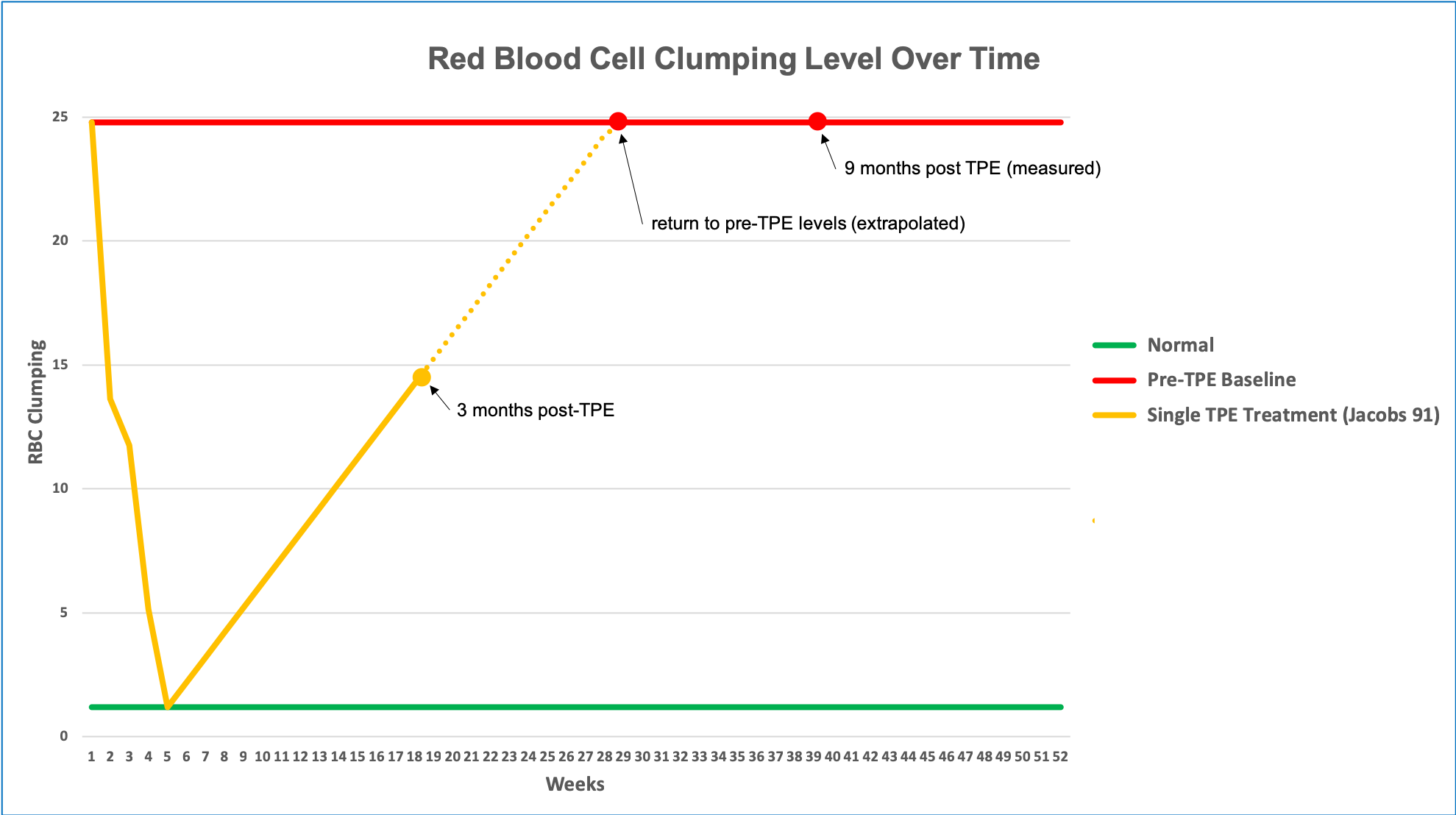
The diagram below shows what happens to red blood cell clumping if you do a series of four weekly TPE treatments, then stop and watch what happens. The green line shows the level of red blood cell clumping in a control group of people without scleroderma. The red line shows the average amount of clumping in the scleroderma group that received the four weekly TPE treatments.
As you can see, even after the first TPE treatment there is a noticeable drop in red blood cell clumping. After four weekly TPE treatments, the red blood cell clumping was completely gone and overall blood viscosity was normal as well. Now notice what happens once TPE is stopped: the viscosity immediately begins to increase again, but does so fairly slowly. Three months later, red blood cell aggregation levels are still only about half of what they were before TPE. At nine months post-TPE, red blood cell clumping was back to pre-TPE levels. Unfortunately, the researchers did not check red blood cell clumping levels between three and nine months after TPE stopped, so we don’t know exactly at what point red blood cell clumping returned to baseline levels.
So now let’s look at what we believe happens if you use our suggested pulsed TPE (one TPE treatment per week for four weeks, wait eight weeks, repeat indefinitely). Eight weeks after the fourth TPE treatment, red blood cell clumping is beginning to return to pre-treatment levels, but is still quite low. As soon as you start the next TPE series, red blood cell clumping levels will immediate begin to fall and should be back to normal again after the fourth TPE treatment in this series, and the cycle starts again.
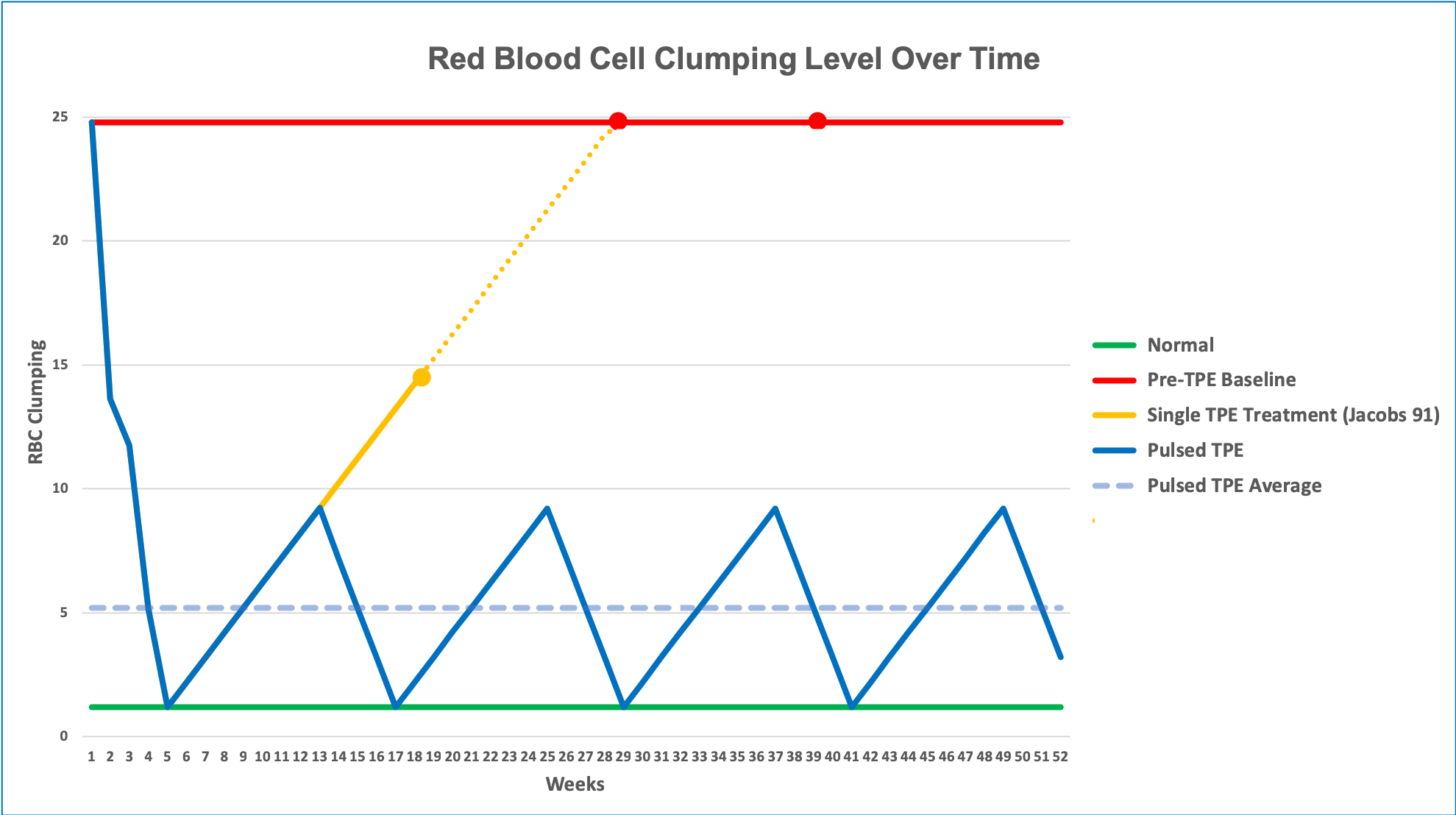
The goal of pulsed TPE is to interrupt the entire disease process at a very early stage before any significant fibrosis or organ damage has occurred. If there is already systemic involvement, the hope is that by preventing the ongoing trauma occurring to blood vessels, disease progression will be halted. With no new disease activity taking place the body may be able to heal to some extent unless organ systems are too severely damaged to recover.
The key and as of yet unanswered question is this: assuming that the overall disease model is correct, which needs to be determined by carefully designed research, what is the level of red blood cell clumping that the body can tolerate before systemic damage starts to occur? In other words, is there a “green zone” where pulsed TPE can prevent further damage and allow people to be mostly symptom free, even though they still have the underlying disease? Pulsed TPE is designed to be a control, not a cure, similar to how insulin can interrupt diabetes or antiretroviral drugs can prevent HIV from progressing to AIDS, even though the underlying disease is still active.
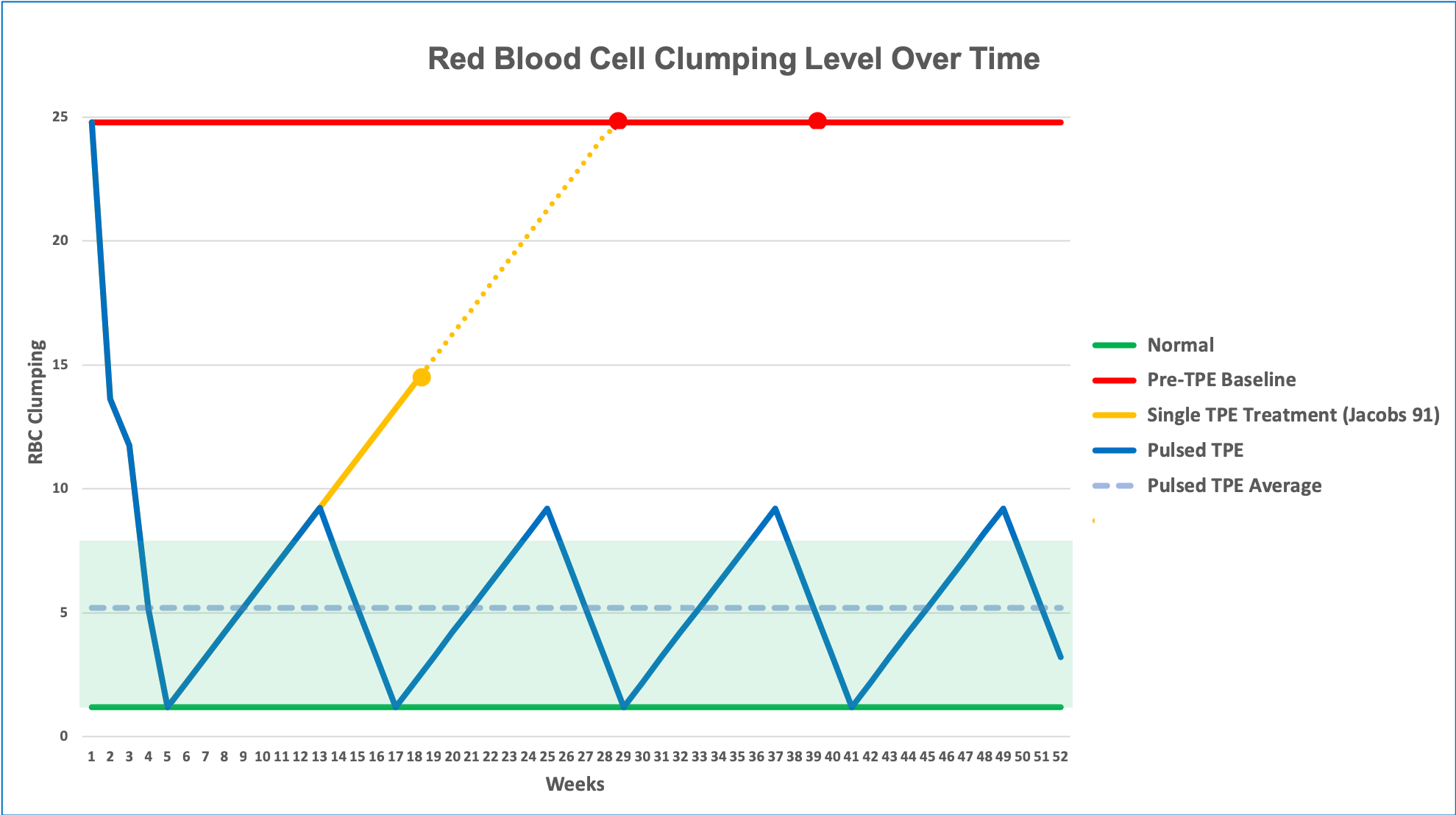
We do have some preliminary data that supports this disease and treatment model. A recently published case report (Harris 2017) followed an SSc patient who has been receiving regular pulsed TPE since 1993 and has been in remission since 1996, including full reversal of all GI symptoms after two years and improvements in lung function over a four-year period. At one point TPE was stopped and the patient started to develop heartburn again about six months later. This reversed once more after returning to the original TPE protocol. The patient does have very mild Raynaud’s and a recent high-magnification nailfold capillary examination showed that the patient has classic early stage capillary damage. This is consistent with the idea that regular pulsed TPE is keeping the patient on the verge of re-developing significant clinical symptoms, but not quite reaching that point.
(One additional note: a second patient is now on the same regular pulsed TPE protocol described in the Harris (2017) paper. She went into full clinical remission after about nine months and is remaining in this status with continued regular pulsed TPE. Her case report is currently under development for future publication.)
Summary
If therapeutic plasma exchange removes an abnormal plasma factor or eliminates the “sludgy” blood characteristics seen in other disorders, thinking about therapeutic plasma exchange as an “oil change” for your body is really a very appropriate metaphor!
References
- Kahaleh MB, Sherer GK, LeRoy EC. Endothelial injury in scleroderma. J Exp Med. 1979;149(6):1326-1335.
- Jacobs MJ, Jörning PJ, Van Rhede van der Kloot EJ, et al. Plasmapheresis in Raynaud’s phenomenon in systemic sclerosis: a microcirculatory study. Int J Microcirc Clin Exp. 1991;10(1):1-11.
- Harris E, Meiselman H, Moriarty P, Weiss J. Successful long-term (22 Year) treatment of limited scleroderma using therapeutic plasma exchange: Is blood rheology the key? Clin Hemorheol Microcirc. 2017;65:131-136. doi:10.3233/CH-16140

First, TPE is a routine procedure used for many different diseases, just not scleroderma routinely. Any large hospital is likely to have the equipment needed for TPE. The issue that patients are encountering is that rheumatologists, in particular, are very conservative and frequently don’t understand TPE since they rarely use it. They often think TPE is not safe (it is much safer than immunosuppressive meds that they routinely order) and that it can’t be done long-term without a catheter or port. In reality, most people can do long-term TPE with just normal venous access (I have done more than 400 TPE treatments since 1993 that way, for example). If you can’t, surgically implanted ports are very reasonable options since they don’t have the infection risk that catheters do.
A few patients are starting to talk to hematologists about trying TPE. Since TPE is associated with abnormal blood rheology such as increased whole blood viscosity and red blood cell clumping, it is something they are comfortable with and understand. TPE is commonly used for hyperviscosity syndromes so they are comfortable using it.
The issue that you are encountering of not being able to get a referral to a scleroderma center is, unfortunately, very common with private insurance. In reality, few general rheumatologists have the training to be able to effectively treat scleroderma patients. They see almost none in routine practice and as a result don’t stay current on diagnosis and treatments.
Is there a medical facility where this TPE specializes with Scleroderma patients? Is the paper/research/ study linked to an Medical University or specialty clinic? I guess that I am asking for these specific reasons:
1. Patient medical coverage options for treatment
2. If treatment is not available locally to patient where could they receive this treatment within a Scleroderma knowledgeable center?
It seems that this is a choice for patients but if your current physician is not on board, how/where can a patient receive this treatment. I understand that research and treatment options must be sought by the Scleroderma patient. It is a must, as the disease is rare, medical info is often outdated and very frightening. But in life 50 hour work week, kids, etc leaves little time for personal research time for a Scleroderma patient. I don’t know if there is an answer but, in my State of MI – my U of M University Rheumatologist will not refer me to the U of M Scleroderma Center. My treatment options are limited as I called the Sclero center at U of M only to be told they would only see me if the U of M Rheum requested it. So I am on my own to find treatment. Where can I get this TPE in a Scleroderma clinic, program, doctor, whatever program I would need?